Eyecare for children
For information on the conditions and what treatment options are available, click through the menu below.
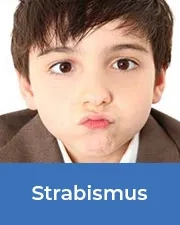
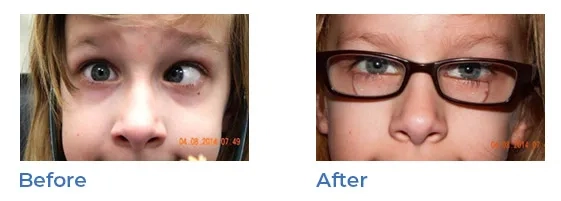
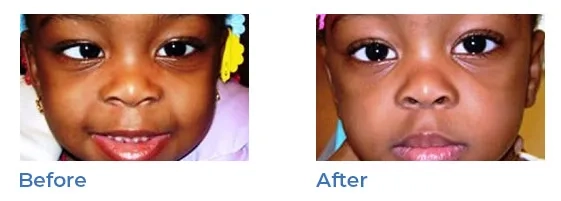
Strabismus
About strabismus
Strabismus, or misaligned eyes, is a condition in which each eye appears to look in a different direction. It is commonly termed 'lazy eyes , ‘misaligned eyes', 'wandering eyes', or 'crossed eyes'. Sometimes, one eye will point straight ahead while the other turns inward, outward or downward.
Strabismus is a common condition among children, affecting four percent of children in the U.S.; it affects boys and girls equally. Although strabismus sometimes runs in families, the exact cause is not fully known.
There are six muscles that control that are attached to the outside of each eye and are responsible for the various movements of our eyes. Strabismus occurs when some of these muscles are not aligned and balanced properly.
Who is at risk?
Since the brain controls these eye muscles, strabismus is more common among children with certain disorders that affect the brain. A child born prematurely, or with other disabilities like cerebral palsy, may be more at risk. Most children with strabismus do not have other problems, but Dr. Wasserman will thoroughly evaluate each child's particular issues.
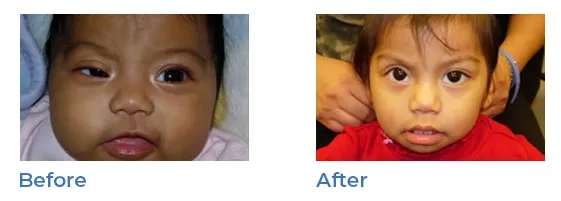
Strabismus treatment
Treatment for strabismus or misaligned eyes involves straightening the eye muscles and attempting to make them work together. If you or your pediatrician suspects your child may have a lazy eye, Dr. Wasserman will conduct a thorough examination. After diagnosis, Dr. Wasserman will recommend the appropriate treatment.
There are several treatment options that can help achieve this:
- Glasses will help straighten the eye
- Eye patching the unaffected eye to help improve vision in the affected eye
- Eye muscle exercises are also suggested for certain types of strabismus. Dr. Wasserman will always take the time to answer all the parents' questions leading to a plan of treatment that can change a child's life.
- Surgery: if the other treatments don’t work, surgery can reposition the muscles in order to rebalance the misaligned eye to balance eye muscles is sometimes the best treatment. Patients sleep through the surgery and go home the same day. During strabismus surgery there is no cutting of the skin, and therefore no scars on the skin afterwards. Dr. Wasserman repositions the eye muscles on the sides of the eye, depending on which direction the eye is misaligned. Sutures are generally dissolvable, and patients go home with eyes open, without need for eye patches. Recovery is usually rapid with most children resuming their normal activities in just a few days.
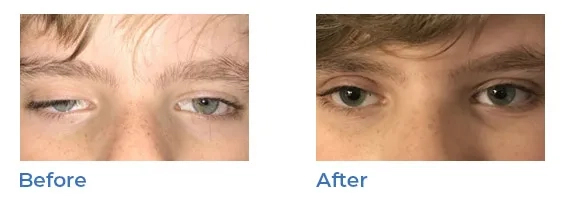
Many adults also have problems with a crossed eye. Some simply never had the condition treated as a child, while in others the condition may have worsened into adulthood. Some adults have had strabismus surgery as a child, but the eyes began to drift again years.
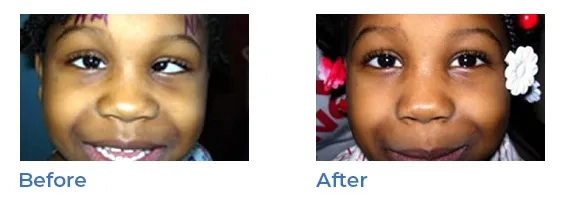

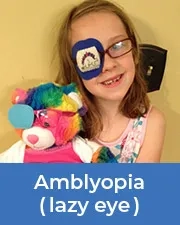
Amblyopia (lazy eye)
The development of equal vision in both eyes is necessary for normal vision. Newborns have some vision, and during the early months vision continues to improve. If a child cannot use his or her eyes in a normal fashion, vision does not develop properly and might even decrease. Amblyopia, or lazy eye, is caused by any condition that affects normal vision development. In some cases, those conditions are inherited. Amblyopia occurs commonly with misaligned or crossed eyes (strabismus). If a child has a significant difference in nearsightedness, farsightedness or astigmatism between the eyes, the blurrier eye can become amblyopic. It can occur in both eyes if both are blurry. Severe forms of amblyopia can be caused by a childhood cataract, or cloudiness in the eye lens.
It is not always easy to recognize amblyopia. Unless the child has a misaligned eye or other obvious abnormality, there is often no way for a parent to tell if something is wrong. If you or your pediatrician suspects that your child has amblyopia, or if there is a family history of misaligned eyes, childhood cataracts, or serious eye diseases, Dr. Wasserman will conduct a thorough eye examination. Using a variety of tests, Dr. Wasserman determines whether one or both eyes are amblyopic. Dr. Wasserman will also carefully examine the interior of the eye for decreased vision, such as cataracts, or retinal or optic nerve disorders.
Once a child is diagnosed with amblyopia, Dr. Wasserman will prescribe a plan that is specific to his or her individual needs. Dr. Wasserman carefully follows the patient over time to be sure there is improvement. Successful treatment of amblyopia depends upon the severity of the problem, and how old the child is when treatment is begun. glasses, patching, and eyedrops, all of which can improve the child’s vision.
Retinopathy of prematurity
Premature infants and their eye issues are another specialty of Dr. Wasserman. Thanks to the incredible, rapid technological advances in neonatal care, an ever-growing number of the smallest premature infants survive the critical first weeks of life. However, with this comes an increased incidence of a vision-threatening eye disease called retinopathy of prematurity (ROP). The disease usually develops in the first few weeks after birth, particularly in those weighing less than three pounds, since they are born before the retina is finished fully developing. The immature retinal blood vessels may grow abnormally during the first months. If the abnormal blood vessel growth becomes severe and is not treated, it may eventually result in retinal detachment and total blindness. Dr. Wasserman is a much sought-after specialist in the area of ROP. He routinely examines the premature babies in the hospital neonatal intensive care units. Rapid progression of ROP demands rapid intervention, and Dr. Wasserman is skilled in the evaluation of the disease. He regularly examines the babies in the neonatal ICU at UMDNJ-Cooper University Hospital in Camden, NJ and St. Peter's University Hospital in New Brunswick, NJ. He also sees many infants in the office for necessary follow up visits after discharge from the hospital. Should an infant progress to the dangerous threshold ROP, treatment is required, and Dr. Wasserman will perform laser surgery.
In order to prevent blindness, sometimes laser surgery is required, along with regular eye exams throughout their life. Children born with ROP The surgery can save the infant from a lifetime of blindness. These infants also require long term follow up. They are also at an increased risk for developing strabismus, glaucoma, amblyopia, retinal detachment and significant refractive errors that can impair their visual development. Dr. Wasserman stays involved with the parents to ensure these children their best chance for good vision into adulthood.
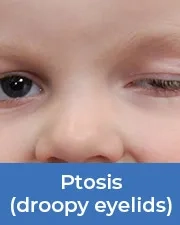
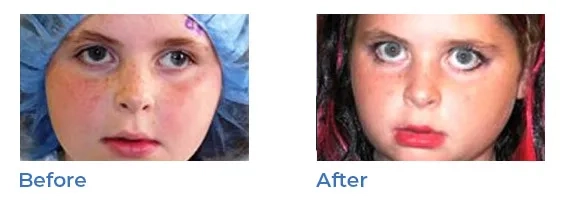
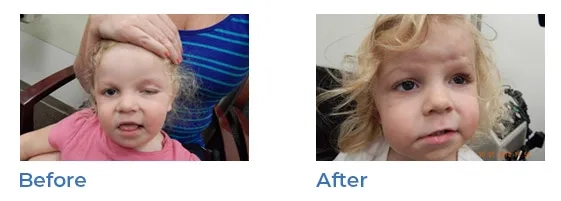
Ptosis (droopy eyelids)
Ptosis, or droopy eyelids can appear at birth or develop over time. A child born with Ptosis may tilt their head in order to be able to see properly. Surgery to shorten the muscle that opens the eyelid can correct the condition. It is recommended around age 5 in order to improve appearance and functionality, making it easier for the child to see.
Dr. Wasserman surgically shortens the muscle that opens the eyelid which accomplishes better vision and improved appearance.
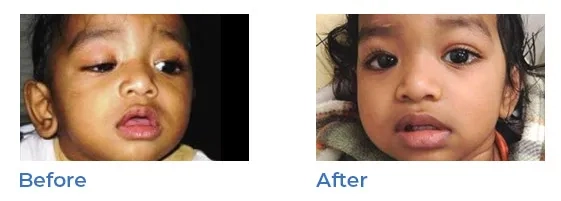
Blocked tear ducts
Blocked tear ducts commonly affects young children. Chronic tearing and mucous discharge can be signs of a blocked tear duct (nasolacrimal duct obstruction). While the tear duct may open without treatment, Dr. Wasserman can cure this problem rapidly and permanently.
Parents are commonly frustrated with constantly wiping away the tears and discharge. Blocked tear ducts can cause the eyelids to become crusted and infections are common.
Dr. Wasserman performs a thorough eye examination and then discusses treatments with the parents. Opening the tear duct is a quick procedure that does not involve any cutting or suturing. Some parents elect to have the baby’s tear duct opened in an office procedure at around six months of age. Others elect to wait until the baby is one year old and have the tear duct opened in a same day hospital procedure.
The procedure is generally very successful, with over 90 percent cured with a single procedure. In some cases, a silicone tube will be temporarily inserted into the tear duct to keep the duct open.
Contact us
If you're in need of any of these treatments, and want to learn more about how Dr. Barry Wasserman can help, please contact us at 609‑243‑8711.
We'd be happy so set up and initial appointment, or simply answer your questions over the phone. We look forward to hearing from you.